A victim of a hit-and-run accident, 21-year-old Samuel Duah, suffered multiple fractures, leading to the amputation of his left arm and leg.
Samuel’s rejection of blood transfusion had led to the rotting away of his badly-injured parts.
His story forms part of hundreds of victims who have lost their lives or function as a result.
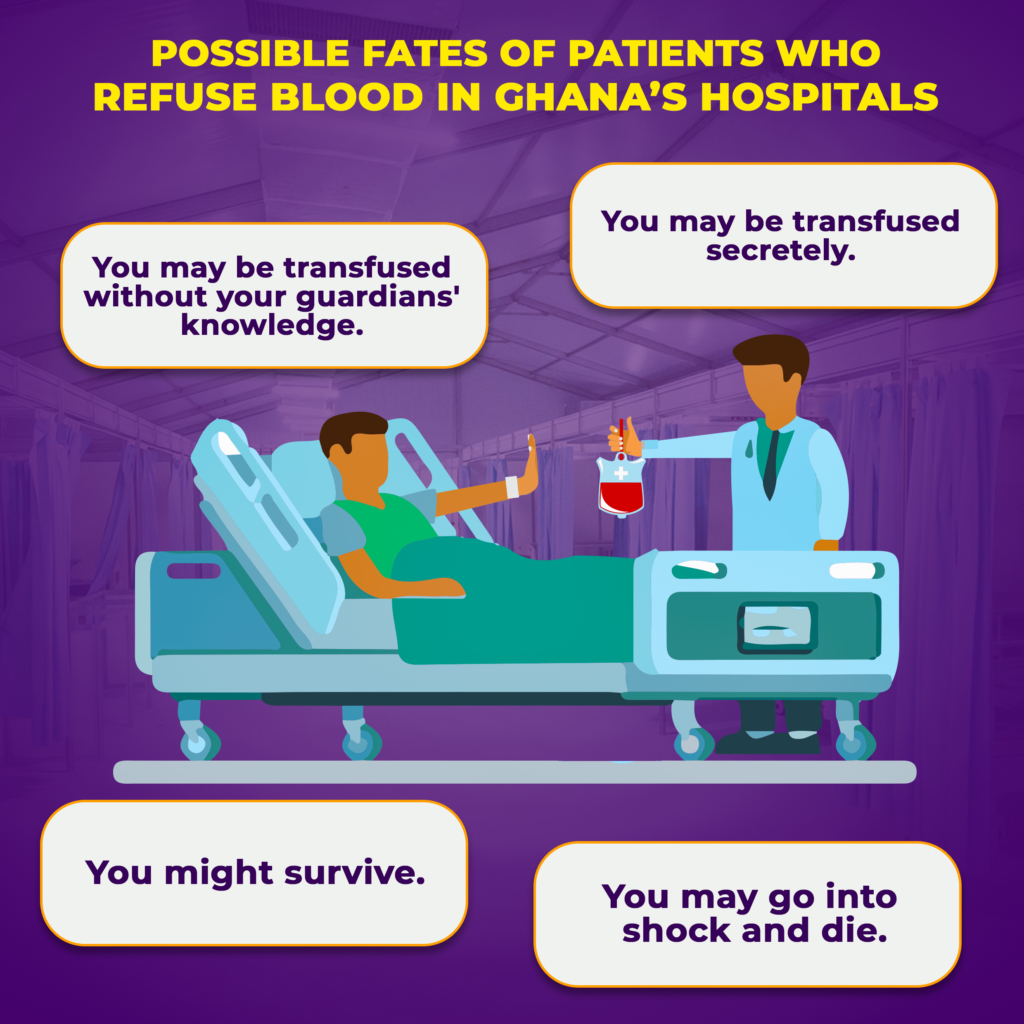
In this report, Medical reporter Denise Akua Owusua exposes the fate of patients who refuse blood, through the surprising accounts of medical professionals, and the alternative treatments available.
It was the third day of his father’s cocoa harvest, and his father and siblings had taken the lead. Accompanied by his friend on his bicycle, he set off to bring them food.
Samuel Duah, a Senior High School graduate had initially planned to search for a job in Ghana’s second largest city, Kumasi. But looking at his septuagenarian father, he rescinded his decision to take up his father’s occupation.
And for a less busy road, Samuel never expected to experience a rear-on collision.
The impact had not only made waste of the bicycle, his legs and arms were not spared.
“My left lower arm and leg and that of my friend’s arms were badly injured. I couldn’t even stand on my feet. The driver, upon seeing us, ran away,” he said.
Luckily, a Good Samaritan took him to the Komfo Anokye Teaching Hospital with extensive injuries to his body, including fractures of the left upper and lower arms, for which reason he had to undergo an above-elbow amputation.
Following the accident and the surgery, he lost a lot of blood. His hemoglobin levels recorded 2.1g/dl, which is medically termed as severe anemia.
The fastest way to correct Samuel’s anemia as a standard protocol in most hospitals is blood transfusion.
The transfusion plan was therefore brought to Samuel and his family to obtain consent, but was however refused, citing religious reasons.
“A few days after the amputation, we were told the left leg was going bad and would need to be amputated as well, but they wanted to first give him blood, which we refused to consent to because we are Jehovah’s Witnesses,” Alice, Samuel’s caretaker affirmed.

Receiving blood
Blood transfusion is the process of transferring safe whole blood or blood products into one’s veins for various medical conditions and to replace lost components of the blood.
The source of the blood may be from another person, or from the same patient obtained earlier and stored for later use.
Common indications for blood transfusion include anemia, which presents as shortness of breath, easy fatigue, palpitations and dizziness. Other indications are acute sickle cell crisis and acute blood loss of more than thirty percent of blood volume.
Blood transfusion can save a patient’s life and limit the complications of severe blood loss, which includes damage to body organs such as the kidneys.
Beyond the strain anaemia imposes on the heart, heart failure could also occur since the heart is not being sufficiently supplied with oxygen.
“Furthermore, blood transfusion prevents the body from depleting its supply of platelets and plasma, which would otherwise result in the loss of coagulation factors and hence, excessive bleeding.
“Blood transfusion benefits patients by treating or preventing these situations,” Dr. Michael Opoku, a general surgeon at Manhyia District Hospital, adds.
On the other hand, much caution is placed on blood transfusion because it predisposes the patient to a tall list of severe side effects.
Firstly, if the blood is not screened properly, the patient is at risk of exposure to various blood-borne infections including HIV, Hepatitis B, Hepatitis C, Syphilis and other bacterial infections.
According to Dr. John Boateng, the founder of Atasemanso Hospital, “The blood-transfused patient is at risk of what is known as hemolytic reactions.
“This condition entails the body fighting against the transfused red blood cells as a result of being incompatible with the donor blood. The situation could cause symptoms such as fever and chills, dizziness, chest pain, lower back pain, bloody urine among others”.
As a result of these possible repercussions of transfusion, such patients typically have an extended hospital stay to ensure such complications are adequately dealt with, should they occur.
A research was conducted in 2014, assessing morbidity and mortality levels in patients with very low postoperative hemoglobin levels, who declined blood transfusion.
The scientists found low risk of mortality in participants whose hemoglobin levels ranged between 7 and 8 g/dl, and a much higher risk for those whose hemoglobin was much lower.
The World Health Organization (WHO) cut off points for anemia are hemoglobin levels less than 11g/dl in adults and less than 12 g/dl in children.
The threshold for transfusion varies from one medical facility or healthcare provider to another.
For most health professionals, such as Dr. Opoku, haemoglobin level below 7g/dl is ideal for blood transfusion.
Samuel’s hemoglobin levels therefore potentially put him in the high risk category.
The hospital therefore decided to manage Samuel with a nutrient medium known as haematinics, which helps in blood production.
But after some days, Samuel’s situation was not getting any better and an amputation of the leg was inevitable.
With Samuel’s refusal of blood transfusion, he had to be discharged.
“They told us they could not proceed with the surgery or do anything else for him if we didn’t consent to the transfusion, so we opted to have him discharged against medical advice,” Alice said.
Health workers at the crossroads
Samuel’s situation adds to the many cases health workers encounter on a daily basis. I therefore sought to find out their experiences and how they dealt with them.
“I did without the parents’ knowledge”
Dr. Aggrey (not his real name for anonymity purposes) recounts an incident where he overrode the parents’ decision and saved a child when he was a house officer.
“A Jehovah’s Witness couple brought their sick child, who was about 3 or 4 years old and subsequently had to be admitted. His Hb was very low and he needed a transfusion but the parents refused. Our attitude towards the parents didn’t differ much even after they refused transfusion.
“The child started deteriorating so we took the child to theatre and transfused without the parent’s knowledge because that was what was in the child’s best interest. After transfusing, the child did much better and was eventually discharged,” he happily told me.
“They recover but slower”
Dr. Esmond Ofori, a senior resident of Obstetrics and Gynecology at the Komfo Anokye Teaching Hospital told me of an encounter with an anaemic pregnant woman.
“I remember one case in question where the patient came in breathless, pale, anemic and we decided to give blood but the patient refused,” he was worried at the time.
“We had no choice but to manage her conservatively with the hope that with time, the body might compensate. We gave her oxygen for several days, parenteral haematinics to build up the Hb at a faster rate and over time, she was weaned off oxygen and her Hb improved as well. Fortunately, she was not actively bleeding. She was eventually discharged,” he said.
A woman who was bleeding heavily was brought to his ward.
“There were others I encountered who were actively bleeding and because they insisted on not taking blood, we managed them with crystalloids and tried as much as possible to stop the bleeding. We did well and eventually, these women recovered.
Dr. Esmond however reveals that in his opinion, their recovery is slower as compared to those given blood.
“Generally in my experience, I would say it is slower compared to those who took the blood.”
“I would say we are more concerned in making sure they don’t decompensate and get worse so we follow up on them.”
“I have not really encountered any patients who have refused blood to the point where they’ve lost their lives. So far, it has not been fatal on my end,” he added.
“One survived but the other sadly died”
Dr. Asamoah, (name modified for anonymity purposes) an Obstetrics and Gynecology specialist recalls:
“A pregnant woman came to us almost at term, with symptomatic anemia; Hb was around 7 and she needed a transfusion. She came along with an advanced directive document indicating she didn’t want blood transfusion. We counseled her on the risks involved, and she understood and stated that she wanted everything that needed to be done aside from being given blood, and if that wasn’t enough and she died as a result, she was ok with it. So we respected her wishes. Fortunately, she did not bleed as much as we anticipated during surgery. Her anemia worsened after delivery but we didn’t transfuse. We gave haematinics and she stayed on admission for almost 3 weeks, the anemia improved and we discharged her.”
In another case, Dr. Asamoah was not able to save the pregnant woman and she eventually gave up the ghost.
“There was this patient referred to KATH from a peripheral hospital with postpartum hemorrhage who refused blood transfusion.
“She was counseled both at the referral facility and here at KATH but she and her husband were firm in their resolve to not take blood transfusion. This woman was very pale so we kept her at our ICU, gave her haematinics. She eventually developed high output heart failure and she was eventually intubated. We kept asking her husband when she lost consciousness if we could transfuse but consent was never given and the woman eventually died,” he said.
“She refused but later agreed and recovered”
A woman who was brought to Dr. Asamoah told him his faith opposed blood transfusion but after several minutes of advice she agreed.
Dr. Asamoah recounted: “There was another case from a referral facility with abruptio placenta that bled significantly with IUFD (intrauterine foetal death) in labour. On her way to KATH, she expelled the foetus. She came to us with severe anemia.
“We were told they belonged to a church opposed to blood transfusion; they were not Witnesses though. Upon further probing, we discovered from the patient that it was her husband who belonged to the church, but not the patient herself so we counseled her and went ahead to transfuse blood and she eventually recovered.”
“She refused, went into shock and died”
In 2008, Dr. Michael Opoku received a middle-aged woman, who had sustained trauma from a road traffic accident.
She needed a below knee amputation of the left lower limb. Because she lost a lot of blood from the injury, she needed blood before the amputation could be done, but she refused it because she was a Jehovah’s Witness.
“So we went ahead with the surgery although her Hb was about 3g/dl.” He said. “Even during the surgery, the patient was in shock and it showed with her BP and pulse rate values.
Though he says they tried all they could, it was not enough to keep her alive.
“We were hoping the plasma expanders we were given would sustain her. Unfortunately, she died on the table.”
“The secretive transfusion kept her alive”
I again chaperoned Dr. Asamoah (name modified for anonymity purposes) back to 2003, where a young SHS student, with an abdominal mass was brought to him.
Unfortunately after surgery, the stitches broke and they had to repair which required blood transfusion.
“We did a right hemicolectomy for her and somehow, the anastomosis broke down so we had to take her back to the theatre to repair it. Her Hb was about 5g/dl at that time so we wanted to transfuse her before that but her mother was a Jehovah’s Witness and so she wouldn’t consent to it.”
Dr. Asamoah continued: “The father on the other hand, was of a different faith so he gave us the consent, however, we did not want to create any issues between the couple so we transfused her at night with the IV bag concealed with a cloth, so the girl herself was not aware of what was happening.”
Eventually, her hemoglobin level built up sufficiently and we were able to take her to theatre and had a successful surgery.
“She is still alive and well today. I think her family always suspected that she got the blood transfusion, but they were generally happy with the outcome of events so nothing more was said or done.”
“She threatened to sue us but was later grateful”
Akosua, a midwife, recalls an incident with a Jehovah’s Witness patient who came with a spontaneous abortion and had bled profusely.
“She arrived semi-conscious and in shock and was rushed to theatre for an emergency evacuation of the uterus (EOU) where she was given blood transfusion,” she began.
”When she recovered, she had to be given blood again and in counseling her for consent, that was when she realized she had already been given blood. She therefore became furious and threatened a court action.”
“She became agitated and threatened to sue the hospital, but upon counseling, she realized she needed the blood, so she consented to it but asked that it be kept from her relatives.”
“So we used to send her to the sideward to transfuse her, and we would tell her relatives she had been taken to the theatre when they came looking for her.”
After the disguised transfusion, she was happy and thanked the health workers who attended to her.
“She improved after receiving 5 units of blood, she was discharged and was very grateful,” she said.
Rights of patients
Samuel is just one of many patients who find themselves at a crossroad when they have to battle between such harsh circumstances and their faith.
According to WHO guidelines, transfusion should be done only when the benefits to the patient outweigh the risks. This goes to show that transfusion is not something that should be taken lightly, and should be relegated as a last resort if possible.
Blood transfusion has consistently been an ethical dilemma amongst medics due to conflicts between morals and claims.
In cases of surgical emergencies, if the person has capacity and refuses blood or blood products, this decision must be respected.
A court deputy does not have the authority to consent to or refuse consent to life saving treatment, even in an emergency.
Dr. Frank Ankobea, the immediate past president of the Ghana Medical Association and legal practitioner has these to say about the ethics of blood transfusion:
“You have to first find out if the patient has a documentation of a prior wish to not accept blood transfusion; this serves as a living will for the patient.
“They may also have a Durable Power of Attorney (DPA) to make decisions on their behalf if they are unable to. A DPA cannot overrule an advanced directive that the patient has documented, nor can they prevent a patient from receiving blood if the patient does not have an advanced directive. This is in the case of an adult.”
“We doctors must realize that the fact that a patient refuses blood transfusion does not mean the patient has refused treatment. It means the patient wants alternatives to be given so they can live. So the patient should not be abandoned just because they refuse blood transfusion.”
“In emergency situations, if the doctor is unaware of any advanced directive document, the doctor can proceed with any lifesaving procedures including blood transfusion.
“If after this, they later discover that the patient has a legal document indicating a wish to not receive blood; it is the responsibility of the health worker to subsequently abide by this. The patient cannot take any legal action for the blood transfusion they received in the earlier instance since the document was not made available.”
“In cases of person’s below 18, the Law is very clear on that. In the Children’s Act Section 8.2, it states that no person can deny a child medical treatment by reason of religious or other beliefs.”
“If the parents are being difficult, the doctor can seek the intervention of the court, so that the court takes the child as a ward of the state.”
“However, there’s a need to be careful in dealing with such issues so that there is no discord created between the child and the parents on account of being given the blood transfusion.”

The uncommon medicine
The Hospital Liaison Committee is a voluntary organization set up by the Jehovah’s Witness Church to minimize any legal or moral conflicts that may arise between Jehovah’s Witness patients and physicians.
They serve as a resource to health facilities and assist them in managing Jehovah’s Witness patients without the use of blood. They also arrange for specific doctor consultations or interventions, and assist in the transfer of patients to other facilities if the current facility is challenged in managing the patient.
The Kumasi Division of the HLC was contacted concerning Samuel’s case, and they assisted by providing alternative medications in lieu of blood transfusion. Subsequently, when KATH faced challenges in managing Samuel’s case due to his refusal to consent to blood transfusion.
Mr. Andrew Abeyie, a pharmacist and member of the HLC Kumasi Division says they provide drugs needed to manage the patient, and restock if there is a shortage in any facility.
“We ensure that we obtain and deliver to any needed location. We also assist families in paying for drugs and treatment if need be. Drugs we provide include erythropoietin, IV Iron, volume expanders and many more.
“The conventional drugs used in hospitals are usually oral iron which works at a much slower rate than the IV iron. We also do presentations at hospitals and provide resources for them as well as a website they can access for updated information.
Mr. Abeyie delineates the HLC has put a system in place to cater for its members.
“Whenever a patient goes to the hospital and there is a situation that requires blood, he’ll inform his church elders, and the elders throughout the region have the contacts of all the 18 members of the HLC, so they contact us on the patient’s behalf.
“Thereafter, we talk directly to the patient, and then speak with the doctor to find out the situation and see what interventions can be done,” he said.
Samuel’s sister, Alice however, recalls instances where drugs supplied by the HLC were ignored by attending nurses.
“They complained they didn’t know how to administer the drugs,” she said.
When Mr. Abeyie was asked why there are still various cases of mortalities related to Jehovah’s Witness patients not accepting blood transfusion, he complained most doctors are not aware there can be bloodless interventions.
“Doctors are well trained in their profession; however, not all doctors have experience in managing cases without the use of blood, which is the conventional method and easier way out.”
Mr. Abeyie observes that sometimes there are delays in managing the patients.
“Some doctors may be hesitant to transfer the patient to another facility. Also, they spend a lot of time trying to coerce the patient to accept the blood transfusion and that can be a problem.
“In healthcare management, delays can cause the death of patients. Sometimes too, the HLC members are not consulted because when we are consulted, then we move in,” he noted.

A study was conducted in 2014 based on forty five adult Jehovah’s Witness patients who underwent bloodless cardiac surgery at Duke University Medical Center between 2005 and 2012.
It showed zero 90-day mortality in the perioperative period. This was achieved using what is called recombinant erythropoietin to increase mean the heamoglobin levels by 1.2g/dl.
Furthermore, a study on the Global Developments in Transfusion Replacements in 2017, details safe evidence-based strategies that are individualized to each patient’s physiology and circumstances. This is collectively known as Patient Blood Management (PBM). It is currently the most viable replacement for liberal transfusion policies.
Prof. Ernest Aniteye, a consultant anaesthesiologist and bloodless medicine expert at the Korle Bu Teaching Hospital, published an article titled “Blood Conservation in Anaesthesia and Surgery”.
Some notable methods of blood conservation methods discussed included autologous blood transfusion, which entails harvesting a patient’s own blood preoperatively over a period of time, when there is a suspected need for transfusion in a pending surgery.
Although this method, known as Preoperative Autologous Blood Transfusion (PABT) is not accepted by the Jehovah’s Witness society, it certainly serves as an acceptable method by other people outside of the faith, who are opposed to blood transfusion.
Indeed, according to a research conducted in Ghana between 1993 and 2003, PABT has become an increasingly popular method at the Korle Bu Teaching Hospital for patients coming for gynecological and orthopedic surgery.
There is, however, what is known as Intra-operative and post-operative blood salvage which involves collecting and processing the patient’s own blood and re-transfusing during surgery. If this is done without a break in the continuity of the circuit, this method is accepted by the Jehovah’s Witness body.
Dr. James Prah, the Deputy Director of health services at University of Cape Coast Hospital, and an expert in bloodless procedures maintains: “I can assure you that bloodless medicine works. We are one of the few facilities in Cape Coast here, who conduct surgeries without blood transfusion.
“Unlike other facilities which require prior blood donation before carrying out surgeries like myomectomy, it’s not a requirement here,” he stated.
Samuel’s bloodless journey
The HLC orchestrated Samuel’s transfer to Atasemanso Hospital in the Ashanti region for further management.
Dr. John Boateng, whose facility nursed him back to health, said he was brought in a very bad state and surgery was carried out on the second day of admission.
“He was weak with a gangrenous left foot which indicated the presence of severe sepsis.
“He came with a referral Hb of 2.6g/dl and we knew with such a low Hb, there was a possibility of high output cardiac failure to compensate for the deficiency of red blood cells. We put him on iron sucrose infusion because oral iron and erythropoietin in such circumstances don’t work,” he explained.
“We also gave him very high doses of erythropoietin: about 40,000 units. On his second day of admission, we sent him to theatre for the amputation of his gangrenous leg,“ he said.
He was however optimistic of good treatment outcomes.
“We’ve had a lot of success with cases like that, and I’ve been doing this for so many years.
“I started when I was a medical student, and I used to cater for Jehovah’s Witness patients who had been discharged from the wards because they had refused blood transfusion.
“With the assistance of some of the nurses who were also Witnesses, we would go to their homes to treat them, and now they’re still alive, even with Hb levels as low as 2g/dl,” he said.
Samuel is currently doing very well at home since being discharged after his second amputation.

A balanced path
Beyond blood transfusion, these promising alternatives can also serve for the greater good of healthcare especially in situations of blood products scarcity.
Dr. Opoku hints: “In my experience, very few people refuse blood and survive, and those tend to be chronic anemia cases, where the body has made compensatory changes. So in such cases, the Hb can be built up slowly. When the blood loss or anemia is acute, they tend not to survive.”
However, Midwife Akosua observes: “I’ve realized most people have a misconception about blood transfusion, not necessarily on religious grounds.
“Some have an issue with it being someone else’s blood and not belonging to their relatives, so they think it’s not good to receive it. But on further counseling, they get to understand and they give their consent to receive it.
“I’ve also nursed patients who stated that even if they are at the point of dying, they do not want to receive blood so we respect their wishes and some of them end up dying with very low Hbs."
Blood transfusion may forever remain a controversial subject largely as a result of its religious implications for some people.
In the midst of the pros and cons of blood transfusion, as well as the alternatives which have undoubtedly saved the likes of Samuel, one must assess and analyze, if no blood truly equates to no life.
Latest Stories
-
Kwesi Atuahene: Ghana’s health capital depends on HealthTech – Africa Center for Digital Transformation
4 mins -
13 signs your wife is planning on leaving you and you have no idea
8 mins -
If I speak there will be fire – Salah on Klopp row
1 hour -
Grieving after divorce is normal, but this particular kind of grief isn’t
1 hour -
10 beautifully unexpected ways husbands proposed to their wives
1 hour -
Reality zone with Vicky Wireko: Painting Ghana purple: Be aware, May is month of mental health awareness
1 hour -
Prof Opoku-Agyemang’s integrity is admirable – Inusah Fuseini
2 hours -
Your reign has been a beacon of wisdom – Alan Kyerematen tells Asantehene
2 hours -
Akufo-Addo’s driver wins La Dadekotopon NPP primary
2 hours -
Education Minister must channel resources to rebrand basic public schools into tackling critical needs – Minority
2 hours -
CAFCC: “Dreams need to score early to unsettle Zamalek” – Former Zamalek striker Felix Aboagye
3 hours -
GHS launches mobile app to counter misinformation about vaccines
3 hours -
Election 2024: Care Ghana warns EC of recruiting political actors as Returning Officers
3 hours -
Mohammed Kudus gets 5th Premier League assist as West Ham hold Liverpool
4 hours -
Religious support source of my success – Asantehene
4 hours

