Anecdotal evidence has recently been reported in the press in Ghana and on social media suggesting a malfunctioning healthcare system in the country leading to avoidable deaths. The demise of 13-year-old Michael Kofi Asiamah (aka Kekeli) stirred up a great deal of negative public sentiments. He was a promising and precocious child whose dreams of becoming a neurosurgeon got shattered by post-surgery complications and events that took his life.
The bereaved mother painfully recounted all the events that led to Kekeli's passing. The doctors did their best to treat Kekeli’s condition [craniopharyngioma], but their efforts stalled in the face of a failed healthcare system. She decried how the “system let [them] down”. In a similar case which resulted in death despite the efforts, two Members of Parliament (MPs) had to make phone calls to some of the big hospitals in Ghana in search of a hospital bed for a 12-year-old boy who had a health emergency.
It appears these unfortunate events represent the daily experiences of many thousands, if not millions, of Ghanaians, most of whom are unable to air their grievances to the general public. To be sure, we decided to look at the relevant data if there will be any supporting scientific evidence. Could it be a baseless claim to link the death cases to the healthcare system?
Could it be that those who do not speak out do not face challenges with their healthcare needs and only a few individuals are affected without the general population suffering? Could it be that, overall, Ghana is not doing too badly as a developing country? In what follows, we answer these important questions with reliable data, show that Ghanaians could have markedly better healthcare outcomes than currently observed, and stress that the healthcare system in Ghana, as it is now, leaves a lot to be desired.
We analyze the socioeconomic data the United Nations used to rank 189 countries in the world in 2020 based on the Human Development Index (HDI). For all these countries, there are data on (1) life expectancy at birth, (2) expected years of schooling, (3) mean years of schooling, and (4) gross national income (GNI) per capita (these are the four sub-components of the HDI). These data are for the year 2019 and are aggregated to rank countries in the world in terms of their level of human development. Ghana ranks 138th out of 189 countries. That means Ghana is generally more developed than only 51 of these 189 countries. Are you impressed?
For the analysis, we focus on life expectancy at birth, which is defined as the average number of years that newborn children are expected to live if current mortality rates and healthcare conditions remain unchanged. Ghana has a life expectancy at birth of 64 years, while most high-income countries have a life expectancy at birth of more than 80 years. As with all data collected and averaged, this does not necessarily mean all Ghanaians will live shorter lives than people in high-income countries. It means a newborn child in Ghana is expected to live about 16 years shorter than a newborn child in a high-income country. Is that fair?
Life expectancy at birth is relatively low in most developing countries because of high child mortality rates (see more details and an interactive map). If most children die before 5, for example, the average life expectancy at birth generally falls drastically. Any weaknesses in the healthcare system and quality of healthcare delivery almost directly affect child health outcomes, as children are usually most vulnerable to health risks. Therefore, life expectancy at birth is an indicator that effectively captures the differences in the quality of healthcare systems and healthcare delivery across countries.
When one compares the performance of Ghana across the four indicators of well-being (i.e. the sub-components of the HDI mentioned above), it turns out that Ghana performs most poorly in life expectancy at birth. As indicated earlier, Ghana is overall more developed than 51 out of 189 countries; but, in terms of health, Ghana is doing better than only 27 countries, which is the worst ranking of all the sub-components of the HDI (see the graphs below or here).
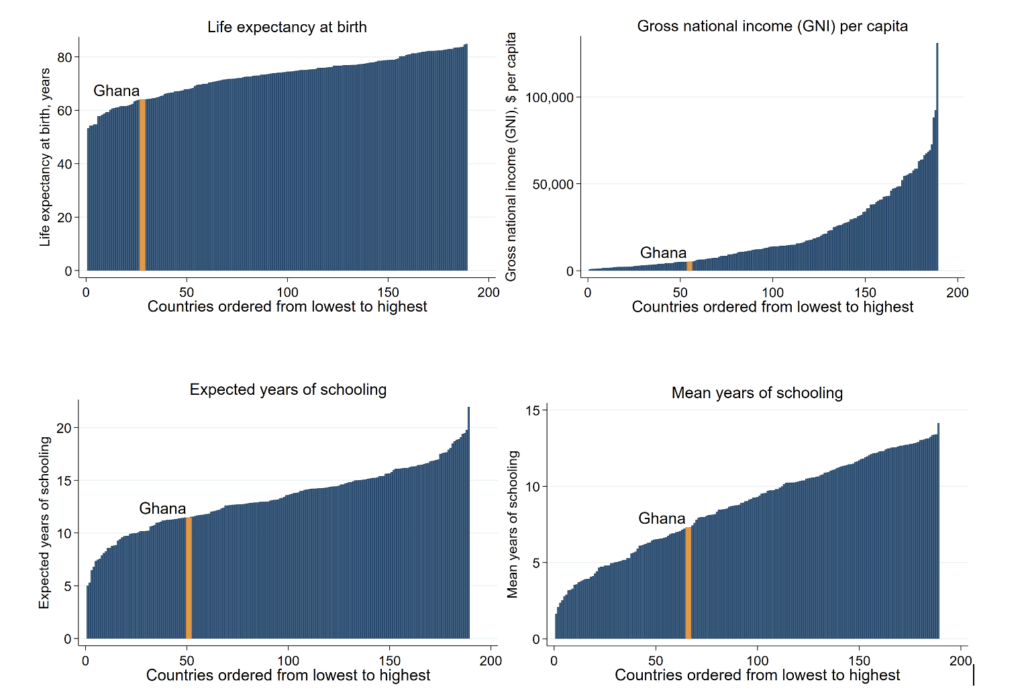
Given Ghana’s performance in the other sub-components of the HDI, can we say that Ghana’s health outcome is disproportionately too low for the country’s overall level of human development? For example, the adult population (i.e. aged 25 or more) in Ghana have spent more than 7 years in school on average, which places Ghana in the bottom 66 countries in the world based on schooling achievements (see the graph in the bottom right), and Ghana is in the bottom 55 countries in the world based on income (see the graph in the top right).
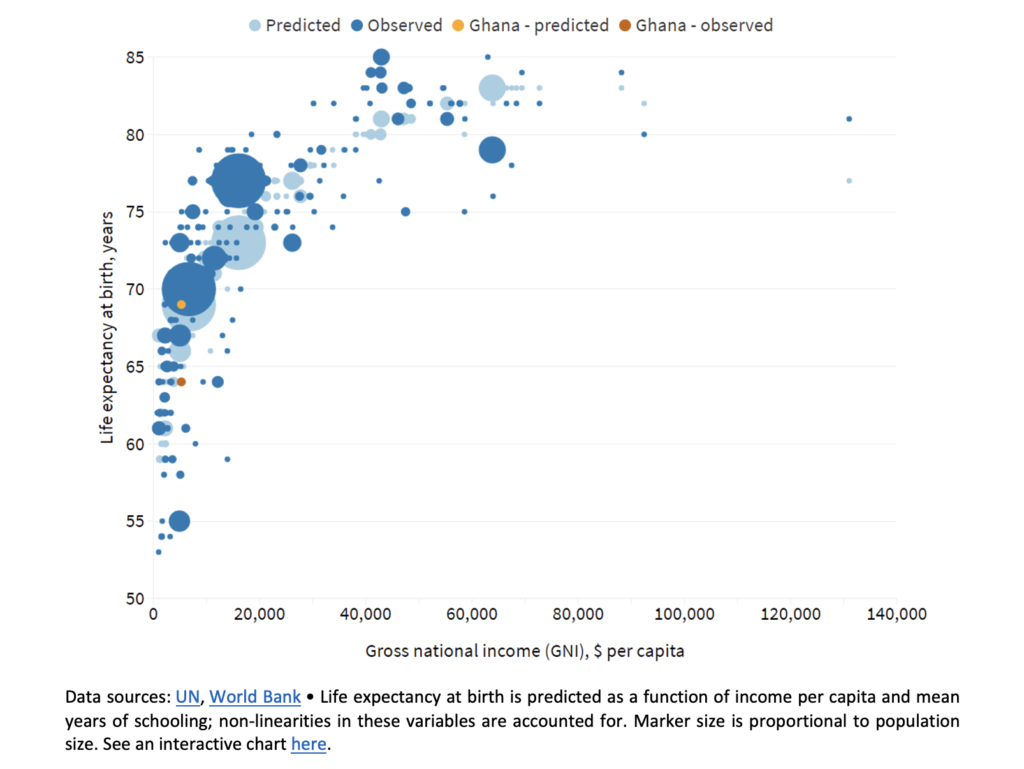
We answer the question we posed above using the strong relationship that exists between life expectancy at birth and income per capita (see Preston, 1975; Deaton, 2013; Deaton and Schreyer, 2020). Richer countries usually have higher life expectancy at birth (see the relationship in the chart below and here for an interactive version). We predict life expectancy at birth conditional on income per capita and mean years of schooling. The main finding is that, even though children born in Ghana could live for 69 years, they are expected to live for only 64 years (i.e. a difference of five years between predicted and observed life expectancy at birth). Ghana is one of only 23 countries in the world where life expectancy at birth is at least five years lower than what one would expect.
Ghanaians should generally live longer and healthier than they currently do if the healthcare system and quality of healthcare delivery were commensurate with overall human development patterns in Ghana and the rest of the world. With this evidence, it is not misplaced to note that healthcare in Ghana is disappointingly poor. Basic medical equipment, such as MRI scanners, CT scanners, and defibrillators, are not readily available in even some of the biggest hospitals in Ghana. This aside, most hospitals are poorly furnished and need to be refurbished to acceptable standards. Medical personnel are scarce, overburdened, and sometimes uncaring and corrupt. Ghana’s healthcare crisis is a real population-wide issue, significant enough to be identified in data representative of the country’s population. Too many Ghanaians are dying or suffering in silence from conditions that could be treated or controlled and thus are living shorter or unhealthy lives without realizing their full potential.
What could be done to improve healthcare outcomes in Ghana is the next big question to be answered. The government may want to prioritize improving the healthcare system and infrastructure. It would be great if the government would increase the share of the total budget committed to the health sector to at least 15% as agreed on in the Abuja Declaration from the country’s recorded average of 8% since the declaration was signed in 2001. We would need more hospitals and clinics, medical equipment, digitized healthcare systems, and personnel in the health sector. It would be key to make working conditions more attractive for healthcare practitioners, including doctors, nurses, paramedics, and technicians, who should be held accountable for their work. The National Health Insurance Scheme (NHIS) should work more effectively to make healthcare services more affordable for all.
The healthcare situation in Ghana is an emergency, yet there is hope as more Ghanaians are becoming more educated and are thus speaking out and calling out for the government to do better. There will be more pressure on the government to allocate more resources for the improvement of health outcomes. It could be a win-win strategy for the present and coming governments to yield to this pressure.
****
We are very grateful for helpful comments we received on earlier drafts of this piece from Ahmed Salim Nuhu, Daniel Gerszon Mahler, Nicole Naadu Ofosu, and Yvonne Goh. We, the authors, are responsible for all errors. We are also personally responsible for all the views presented in this article; we do not represent the views of the organizations we work for.
Latest Stories
-
Drake: AI Tupac track gone from rapper’s Instagram after legal row
1 min -
Repainting schools, changing uniforms a misplaced priority – Joy FM listeners on rebranding of basic public schools
6 mins -
UEFA U-16 Tournament: Black Starlets bounce back with 5-1 win over Serbia
25 mins -
There’s nothing strange about changing colours for basic public schools – Education Ministry PRO
36 mins -
Diana Asamoah causes arrest of personal assistant over GH₵4k MoMo theft
48 mins -
Our mindset should breed excellence – Ace Ankomah
1 hour -
SML fully delivered on Transaction Audit Service Agreement with GRA
1 hour -
Government trying to hide something from SML/GRA contract – Arthur Kennedy
1 hour -
Don’t encourage lateness and foolishness – Ace Ankomah to UG Vice Chancellor’s award winners
2 hours -
‘Obroni wawu’ traders plan to protest over Kumasi Central Market Redevelopment delays
2 hours -
Gold Fields Ghana boosts cocoa production in Huni Valley District through Cocoa Farmers’ Support programme
2 hours -
Spanish government to oversee football federation after Luis Rubiales scandal
2 hours -
TikTok will not be sold, Chinese parent tells US
2 hours -
Bawumia is ready to announce his running mate – Miracles Aboagye
2 hours -
Works and Housing Ministry launches BENCHH 2024
2 hours

