Audio By Carbonatix
Recently, a patient of mine came to clinic with a new cough and shortness of breath.
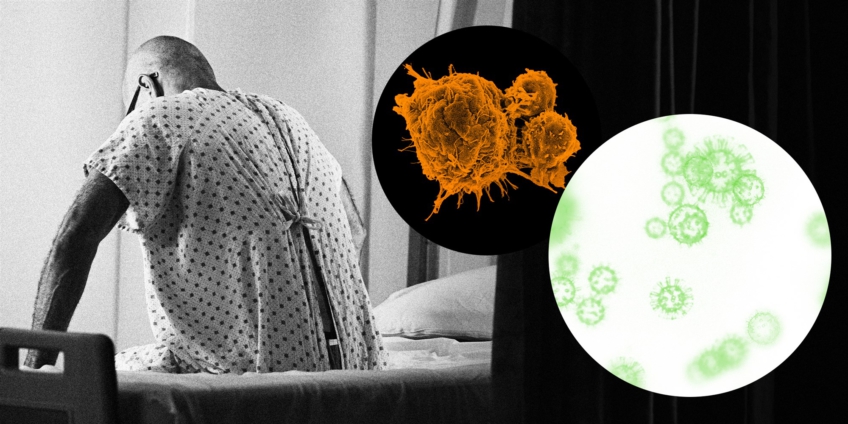
Though I was already treating him for stage 4 colon cancer that had studded his lungs, his acute symptoms made me even more concerned about Covid-19.
Tragically, he died the next day as the coronavirus easily overpowered an immune system neutered by cancer and chemotherapy.
Almost one year into the pandemic, many of the fears harbored by oncologists like me have been fully realized in clinical practice.
Apart from felling scores of cancer patients, the virus has upended cancer diagnosis, treatment and research.
Covid-19 attacks the lungs, of course, but it also disrupts other organs — and really, entire health systems.
By now, Covid has been linked to heart disease, diabetes, stroke, low blood cell counts and psychiatric conditions.
Cancer patients possess little resistance against Covid-19. The older you get, the higher your cancer risk.
But advanced age is also a risk factor for coronavirus.
Metabolic disorders associated with cancer, like obesity, high blood pressure and diabetes, add further vulnerability.
A study in the JCO Global Oncology journal examined how patients diagnosed with Covid-19 during the early portion of the pandemic fared in Asia, Europe and the United States.
It showed that patients with cancer had worse outcomes (greater need for ICU admission and higher mortality) than those without cancer.
Based on data from the United Kingdom, an analysis published in Nature found that a Covid-19 infection within the first year of a cancer diagnosis was especially lethal.
Compared to those without cancer, patients with a solid organ cancer (e.g., breast, lung and colon) had 1.8 times the risk of death, while those with a blood cancer had a fourfold greater risk.
And unfortunately, the results of a recent University of Pennsylvania study show that even those whose cancer is in remission and who are not currently requiring any therapy remain prone to severe Covid-19 infections.
As Nathan Berger, a professor and oncologist at Case Western Reserve School of Medicine recently told STAT News: “The combination of the virus and cancer is synergistic and leading to mortality. The death rates are much higher than they are for either of the diseases alone.”
Yet even those cancer patients who avoided direct infection could not entirely escape the coronavirus’ seismic effect on health care systems.
As health care resources were reallocated to the pandemic response, staple treatments such as elective cancer surgery and radiation were deferred, while systemic therapies like chemotherapy were delayed.
In cancer, time is exceedingly precious.
A study in the British Medical Journal found that even a four-week delay in cancer treatments caused an uptick in mortality for seven different cancers, including breast, lung and colon.
Routine screenings for cancers of the breast, cervix and colon also nosedived during the pandemic due to insurance issues or fears of contracting Covid-19 from health care facilities.
Last year, these screenings were down more than 90 percent when compared to previous years.
Though the full impact of these missed or delayed colonoscopies and mammograms hasn’t registered yet, it is possible — likely, even‚ that many preventable or early stage cancers were simply missed.
As William Cance, chief medical and scientific officer of the American Cancer Society, grimly told The Wall Street Journal, “We undoubtedly will have delays in diagnoses, and more advanced cancers.”
Research trials that blaze new trails and possibilities for cancer treatment have also been scuppered by lockdowns and dwindling recruitment.
Given that cancer remains the second-leading cause of death in America and is only expected to increase due to rising life expectancy and exposure to risk factors, the new drugs and therapies unearthed through trials are critical.
Oncologists like myself feel the weight of Covid-19’s daily interference in our patients’ cancer care.
Any unexplained fever, cough or vague symptom in a patient now compounds concerns and adds an additional layer of paranoia, risk and complexity.
Unsurprisingly, oncologists have reported a surge in their personal anxiety and depression during the pandemic.
Though the ongoing vaccine rollout offers hope, it is fraught with uncertainty.
Like so many gray areas surrounding Covid, it is unknown whether an immunocompromised cancer patient can mount a sufficient immune response to vaccination.
But even a diminished benefit from the vaccine will add some armor against the virus’ spike protein.
From diagnosis and beyond, the fate of many cancer patients is now tied closely to the contagion’s trajectory.
Latest Stories
-
Airport renaming doesn’t require parliamentary approval—Transport Minister
12 minutes -
Renaming of airport will not impose huge cost on state – Transport Minister
15 minutes -
Standard Chartered hosts business roundtable on capital markets
23 minutes -
Cocoa price reduction: Clerks cry over attacks by farmers, describes reduction as scam
27 minutes -
Cedi recovers modestly on external tailwinds; one dollar equals to GH¢11.70 at forex bureaus
32 minutes -
Acute water shortages hit Kumasi as power outages cripple Barekese, Owabi plants
38 minutes -
Accra Mayor calls on businesses to prioritise PWDs and youth in recruitment
40 minutes -
40 Ghanaian languages at risk as GhLA calls for urgent preservation
43 minutes -
Ghana Energy Awards opens 10th anniversary activities with courtesy call on Ministry
44 minutes -
Medikal’s “Beyond Kontrol” concert at Accra Sports Stadium earns IRAWMA nomination
47 minutes -
Daily Insight for CEOs: Leadership Resilience under Pressure
48 minutes -
First British baby born using transplanted womb from dead donor
51 minutes -
GRIDCo investigates fault that caused power outage in parts of Tema
57 minutes -
Ahanta West Assembly members dissociate from petition against MCE
58 minutes -
“Success must be seen on the grounds, not just in policy documents” – Sports Fund chairperson
59 minutes