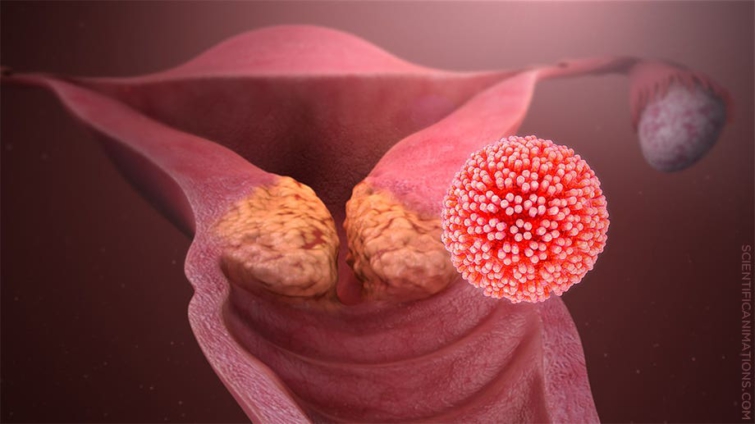
Cervical cancer is cancer of the cells of the cervix. The cervix is the mouthpiece and the doorway into the womb (the part of the female reproductive tract, which accommodates the unborn baby).
World Health Organization (WHO) affirms that cervical cancer is the 4th most common female cancer worldwide with 604,000 new cases with 342,000 deaths recorded annually which means over half of the cases leads to deaths. This is mainly due to late detection because of low turn-out rate for screening and preventive measures.
Cancer takes a while to manifest with symptoms. Many cancers do exist but only a few have a definite cause: gastric cancer caused by helicobacter pylori and cervical cancer caused by human papilloma virus (HPV). Avoidance, riddance and prevention of these infections eliminate the above stated cancers. This is why they are entirely preventable.
For other cancers like breast, prostate and lung cancers, etc. we do not have an identifiable cause. They just have recognizable risk factors which increase their probability of occurrences if the associated risk factors are present in the individual.
Avoidance, riddance and prevention of the risk factors only reduce the probability of developing these cancers (that is increases the time taken to develop cancer if you’ll develop it before death or you never develop it at all).
Causes and risk factors
The main established cause of cervical cancer is the oncogenic human papilloma virus (HPV), an incurable sexually transmitted infection(STIs). Oncogenic meaning cancerous HPV; types 16&18. This is because not all HPV types of infection lead to cancers; HPV type 6 and 11 causes genital warts (condylomata accuminatum).
HPV is the most common viral STI worldwide. More common than HIV. Currently, HIV cases stand at 25,789cases in Ghana according to Ghana Aids Commission(GAC) as of 27th January, 2022. If HPV is commoner than HIV, do the math; more HPV infection numbers isn’t it?
About half of the HPV cases are between 15-24yrs The only way it is gotten rid off, is by the soldiers of our body (immune system) doing away with it naturally in about 90% of HPV infections purported by WHO and not through a curing drug.
The risk factors of cervical cancer include female gender, older age (>35yrs), having multiple sexual partners, early sex (<20yrs), unprotected sex, alcohol drinking, smoking, HIV infection, chronic steroid use.
The presence of the risk factors will hasten the development of the cancer if the HPV is present. In the absence of the risk factors, it take 15-20yrs for HPV to develop into the cervical cancer in a normal immunocompetent female.
The young person(25yrs) is most susceptible to the infection. This is because, the part of the cervix susceptible to the brunt of the HPV infection is broadly exposed but after 25yrs through nature, growth, development and hormonal changes of the female genital tract, it is obscured even when the HPV infection is present.
This is why you need to be responsible by abstaining, sticking to one sexual partner whom you can predict his/her sexual escapades or use a condom.
Signs and symptoms
The symptoms of cervical cancer can be grouped into either early or late symptoms. Early symptoms include vaginal bleed in a postmenopausal female, vaginal bleed after sex (postcoital bleed) in a non-virgin (hymen break may cause bleeding after sex in a virgin and that isn’t cervical cancer), any vaginal bleed not in concordance with menses, bloody spot stains in your underwear, persistent vaginal discharge that may be foul smelly.
Late symptoms are often severe which include persistent back or leg pain, pelvic pain(waist level pain), loss of appetite with weight loss and a foul smelly vaginal discharge. Any one of a combination of a few should prompt the sufferer to go see the gynaecologist, especially the early signs.
Get tested
Interacting with a number of females, they complain that they have reservations against the pap test (Papanicolaou test) and that’s what bars them from going for the test although they know how beneficial it is. They complain that it is uncomfortable.
Now there is a way out. Let me brighten your day. Previously, a pap test was always done for every female for screening. The narrative has changed in that not all females need a pap test for cervical cancer screening. A preliminary self user-friendly home kit can be used. It is used but only >29 yr old females for screening. Depending on the results, a pap test is mandatory to establish a cervical cancer diagnosis. Testing is for both vaccinated and unvaccinated ladies.
Prevention
Abstinence, be faithful, refraining from quickies and one night sex with complete strangers you know little about their sexual expeditions. Rather use a condom. Vaccination is primary prevention available to people between the ages of 15-25yrs also offers nearly 100% protection for 10years.
Vaccination is not for free. I want to use this platform to appeal to policy changers to make vaccination free. Doing away with the above risk factors also offer some protection.
Treatment
Treatment is individualized and depends on the patient with her relatives, and the stage of the disease in consultation with their gynaecologists. She may be advised to choose chemotherapy or radiotherapy or surgery or a combination of any of the 3 or all.
Dr MICHAEL BAAH BINEY
(@_papabiney on twiiter & Instagram)
Ghana Medical Association Member
Global Health Head @ Kandifo Institute
mikebiney77@gmail.com
Latest Stories
-
Paris 2024: Opening ceremony showcases grandiose celebration of French culture and diversity
3 hours -
How decline of Indian vultures led to 500,000 human deaths
4 hours -
Paris 2024: Ghana rocks ‘fabulous fugu’ at olympics opening ceremony
4 hours -
Trust Hospital faces financial strain with rising debt levels – Auditor-General’s report
5 hours -
Electrochem lease: Allocate portions of land to Songor people – Resident demand
5 hours -
82 widows receive financial aid from Chayil Foundation
5 hours -
The silent struggles: Female journalists grapple with Ghana’s high cost of living
5 hours -
BoG yet to make any payment to Service Ghana Auto Group
5 hours -
‘Crushed Young’: The Multimedia Group, JL Properties surprise accident victim’s family with fully-furnished apartment
6 hours -
Asante Kotoko needs structure that would outlive any administration – Opoku Nti
6 hours -
JoyNews exposé on Customs officials demanding bribes airs on July 29
7 hours -
JoyNews Impact Maker Awardee ships first consignment of honey from Kwahu Afram Plains
8 hours -
Joint committee under fire over report on salt mining lease granted Electrochem
8 hours -
Life Lounge with Edem Knight-Tay: Don’t be beaten the third time
8 hours -
Pro-NPP group launched to help ‘Break the 8’
8 hours